Ascites secondary to Chronic liver disease
This is an online e-log book to discuss our patient's de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss individual patients' problems through a series of inputs from an available global online community of experts with an aim to solve those patients' clinical problems with collective current best evidence-based input.
This E blog also reflects my patient-centered online learning portfolio and your valuable input in the comment box are welcome.
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, and investigations, and coming up with diagnosis and treatment plan
The patient/attender was informed of the purpose of the information being acquired. Informed consent was taken from the patient/attender and there is the omission of information that was requested to be omitted.
P Sri Sai Sanjana
2019
Roll No: 96
DEMOGRAPHICS:
Age: 39 yrs
Gender: Male
Occupation: Cab driver
Address: West Bengal
CHIEF COMPLAINTS:
A 39-year-old male came with chief complaints of:
- Abdominal distention since 2 months
- Bilateral pedal edema since 2 months
- Decreased appetite since 2 months
- Decreased urine output since 1 month
HISTORY OF PRESENTING ILLNESS:
The patient was apparently asymptomatic 2 months back. Then he developed abdominal distention which was insidious in onset, gradually progressive, and associated with decreased appetite.
Bilateral pedal edema extending up to knee since 2 months, pitting type, increased on walking and relieved with rest.
Decreased urinary output since 1 month
No h/o fever, cough, breathlessness
No h/o pruritus, blood in vomiting and stools
PAST HISTORY:
No h/o DM, HTN, TB, asthma, epilepsy, CVA. CAD
PERSONAL HISTORY:
- Diet - mixed
- Appetite - decreased
- Sleep - adequate
- Bowel and bladder movements - regular
- Consumes alcohol -180ml
- Stopped consumption of alcohol from the day of admission
- Smokes beedi 1 pack per day and stopped 3 months back
Daily routine:
Patient wakes up at around 5:00 am every day and freshens ups. Have a cup of tea then at around 9 am has his breakfast (rice and dal). He goes cycling to his workplace. Then he will have his lunch at 1:00 pm and then comes back home around 9:00 pm. He then has dinner, consumes alcohol and goes to bed at 10:00pm.
Alcohol consumption is usually on alternative days.
GENERAL PHYSICAL EXAMINATION:
The patient is conscious, coherent, cooperative, and well-oriented to time, place, and person.
Moderately built and nourished.
Pallor - absent
Icterus - absent
Cyanosis - absent
Clubbing - absent
Generalized Lymphadenopathy - absent
Edema - Bilateral pedal edema, pitting type
VITALS:
Temperature - afebrile
PR: 95bpm
RR: 22cpm
BP: 110/70mm Hg
SYSTEMIC EXAMINATION
Per abdomen-
Inspection-
Abdomen is distended, flanks are full, skin is stretched, umbilicus is everted, no visible peristalsis, equal symmetrical movements in all quadrant’s with respiration, no dilated abdominal veins
Palpation-
No local rise of temperature, no tenderness
All inspectory findings are confirmed by palpation, no rebound tenderness, guarding and rigidity
No tenderness, No organomegaly
Fluid thrill present
Percussion-
Shifting dullness present — dull note is heard from the level of umbilicus
Auscultation-
Bowel sounds heard
CVS: S1 and S2 heart sounds heard, no murmurs
CNS: No focal neurological deficits
RR: BAE Present, normal vesicular breath sounds heard, no adventitious sounds, shape of the chest: normal, trachea appears to be central
Ascitic fluid
Appearance - clear, yellow coloured
SAAG - 1.65 g/dl
Serum albumin - 2.0 g/dl
Asctic albumin - 0.35 g/dl
Ascitic fluid sugar - 104mg/dl
Ascitic fluid protein - 0.7 g/dl
Ascitic fluid amylase - 17 IU /L
LDH : 143 IU/L
Cell count- 50 cells
Lymphocytes nil
Neutrophils 100%.
Chest x-ray
Fever Chart
USG abdomen
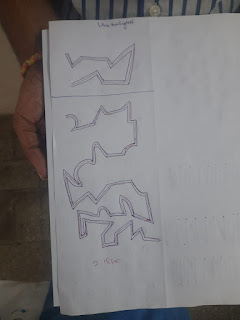
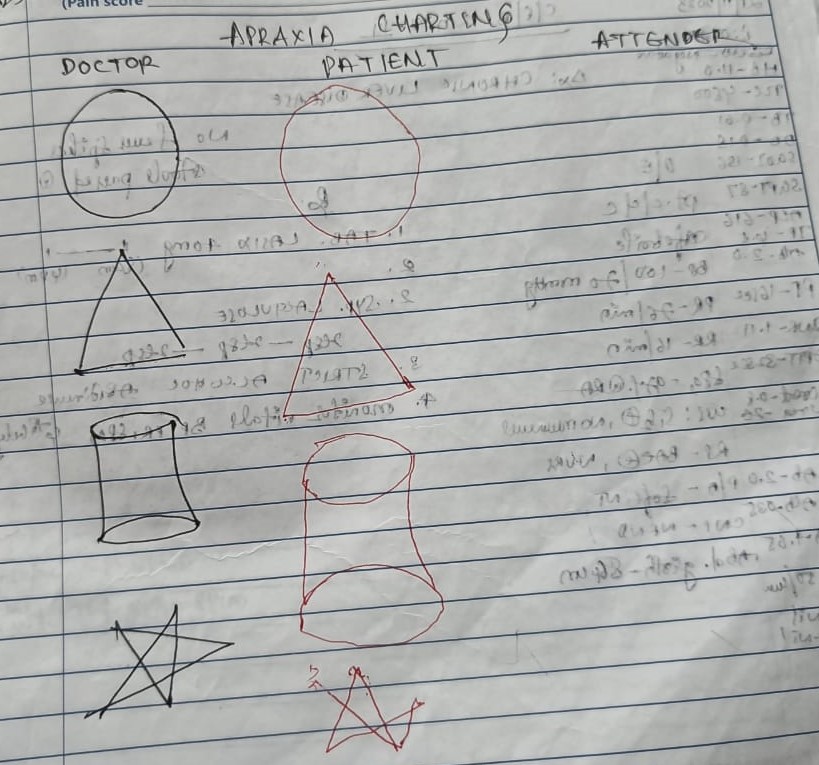
PHES test
Interpretation
INVESTIGATIONS:
30/11/23
Ward-9
Admission date- 16-11-23
S - No fever spikes, Stools passed
O - Patient is conscious, coherent, cooperative
Vitals-
BP - 100/60mmhg
PR - 74bpm
RR - 16cpm
SpO2 - 98%
Temperature - afebrile
CVS-S1 &S2 heard, no murmurs
RS - BAE+ ,NVBS
P/A - Soft, Distended, abdominal girth - 86cm; weight - 46kg
CNS - No focal neurological deficits
A- Ascites secondary to chronic liver disease
P- Tab Lasik 20mg
Syrup lactulose 15ml
Zecof cough syrup 5ml TID
Strict alcohol abstinence
Monitor vitals & inform SOS
1/12/23
Ward-9
Admission date- 16-11-23
S - No fever spikes, Stools passed
O - Patient is conscious, coherent, cooperative
Vitals-
BP - 110/70mmhg
PR - 76bpm
RR - 17cpm
SpO2 - 98%
Temperature - afebrile
CVS-S1 &S2 heard, no murmurs
RS - BAE+ ,NVBS
P/A - Soft, Distended, abdominal girth - 86cm; weight - 46kg
CNS - No focal neurological deficits
A- Ascites secondary to chronic liver disease
P- Tab Lasik 20mg
Syrup lactulose 15ml
Zecof cough syrup 5ml TID
Strict alcohol abstinence
Monitor vitals & inform SOS
TREATMENT:
Tab LASIX 20 mg PO OD
Syp. Lactulose 15 ml PO TID
Zecof Cough Syrup 5 ml PO TID
Strict Alcohol abstinence
EDUCATIONAL POINTS: